
Aktuelles

Willkommen auf unserer neuen Homepage!
Wir laden Sie herzlich ein, unser Profil beim Durchklicken kennenzulernen! Laufende Meldungen gibt es auch auf Instagram.
Weiterlesen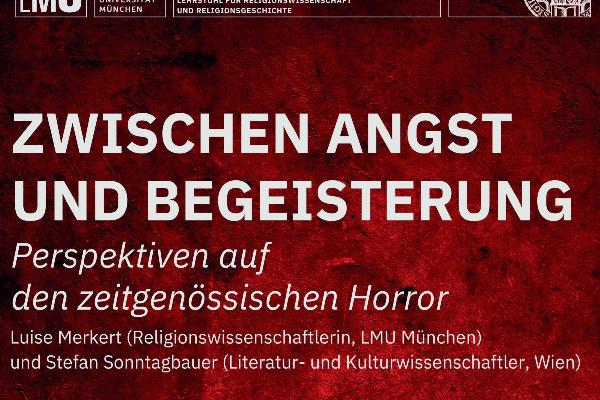
Interdisziplinäres Blockseminar im SoSe 2024
Für die einen ein unverzichtbares Medium für den Adrenalinkick, für die anderen ein Albtraum, der die allgemeine Abstumpfung vorantreibt. Kein Zweifel, bis heute wird kein anderes Genre so heftig diskutiert wie der Horror.
Weiterlesen
Theologie studieren
Ein Film des BR zum Theologiestudium an der Evangelisch-Theologischen Fakultät der LMU.
WeiterlesenDie evangelische Theologie beschäftigt sich mit den zentralen Motiven des Christentums, ihren biblischen Wurzeln, ihrer historischen Entwicklung und ihrer Bedeutung für unsere Gegenwart. Unsere Fakultät bietet Gelegenheit, eine der ältesten und interessantesten akademischen Disziplinen der europäischen Geistesgeschichte an einer der besten Universitäten und in einer der schönsten Städte Deutschlands zu studieren. Wir freuen uns auf Sie.Professor Dr. Jörg Lauster, Dekan



